Hipertensi Pulmonal Kenali Gejala Awalnya
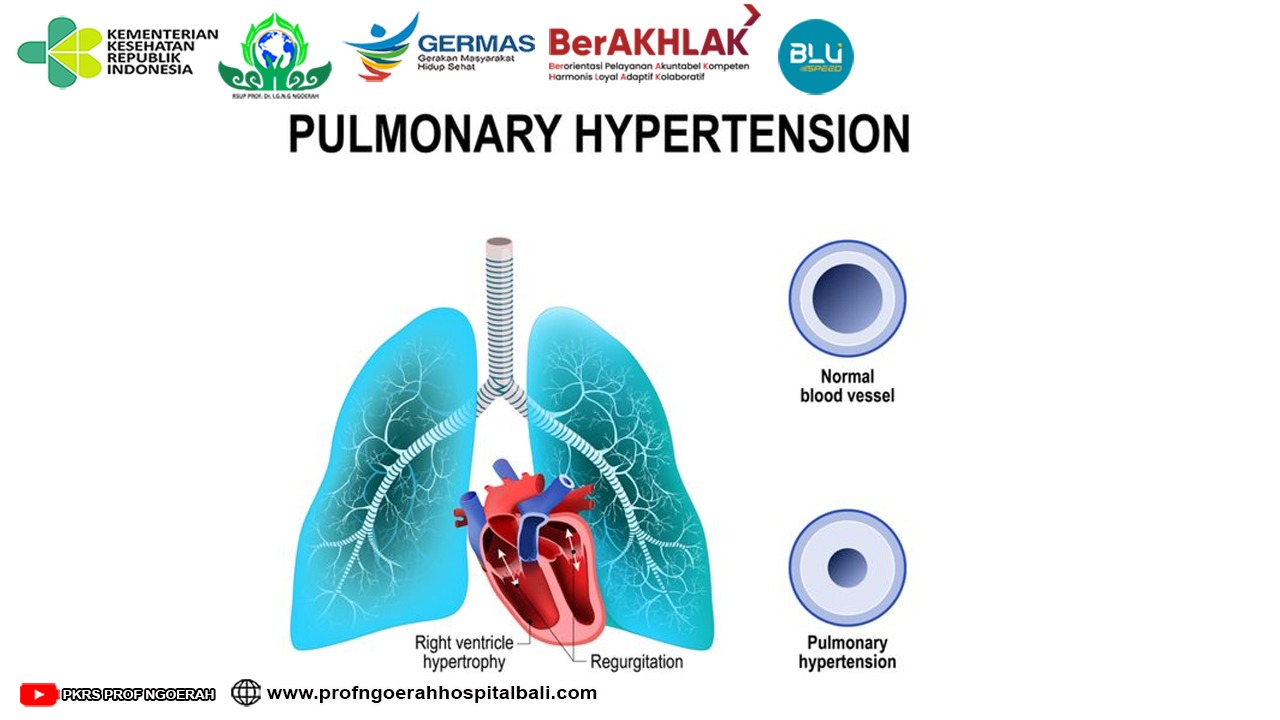
Hipertensi pulmonal (HP) adalah manifestasi hemodinamik dari berbagai proses patologi yang menyebabkan peningkatan tekanan arteri pulmonal (mPAP) >25 mm Hg, mean pulmonary wedge pressure, left ventricular end diastolic pressure kurang dari 15 mmgHg dan pulmonary vascular resistance >3 wood units <!--[if supportFields]>ADDIN CSL_CITATION { "citationItems" : [ { "id" : "ITEM-1", "itemData" : { "ISSN" : "1178-2005", "PMID" : "19802350", "abstract" : "Pulmonary hypertension (PH) is the hemodynamic manifestation of various pathological processes that result in elevated pulmonary artery pressures (PAP). The National Institutes of Health Registry defined pulmonary arterial hypertension as the mean PAP of more than 25 mm Hg with a pulmonary capillary wedge pressure or left atrial pressure equal to or less than 15 mm Hg. This definition remains the currently accepted definition of PH that is used to define PH related to multiple clinical conditions including chronic obstructive pulmonary disease (COPD). The estimated US prevalence of COPD by the National Health Survey in 2002 in people aged >25 was 12.1 million. There is a lack of large population-based studies in COPD to document the correct prevalence of PH and outcome. The major cause of PH in COPD is hypoxemia leading to vascular remodeling. Echocardiogram is the initial screening tool of choice for PH. This simple noninvasive test can provide an estimate of right ventricular systolic and right atrial pressures. Right heart catheterization remains the gold standard to diagnose PH. It provides accurate measurement of mean PAP and pulmonary capillary wedge pressure. Oxygen therapy remains the cornerstone therapeutic for hypoxemia in COPD patients. Anecdotal reports suggest utility of PDE5-inhibitors and prostacyclin to treat COPD-related PH. Large randomized clinical trials are needed before the use of these drugs can be recommended.", "author" : [ { "dropping-particle" : "", "family" : "Jyothula", "given" : "Soma", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Safdar", "given" : "Zeenat", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" } ], "container-title" : "International journal of chronic obstructive pulmonary disease", "id" : "ITEM-1", "issued" : { "date-parts" : [ [ "2009", "1" ] ] }, "page" : "351-63", "title" : "Update on pulmonary hypertension complicating chronic obstructive pulmonary disease.", "type" : "article-journal", "volume" : "4" }, "uris" : [ "http://www.mendeley.com/documents/?uuid=235c9742-9c2a-4525-9513-679b801ca99b" ] } ], "mendeley" : { "previouslyFormattedCitation" : "(2)" }, "properties" : { "noteIndex" : 0 }, "schema" : "https://github.com/citation-style-language/schema/raw/master/csl-citation.json" }<![endif]-->(1,2)<!--[if supportFields]><![endif]-->. Keadaan ini dengan gejala yang khas sering menyebabkan gangguan pada beberapa sistem, misal saja pada pasien dengan penyakit paru obstruktif kronik ( PPOK) yang lama. Penyakit paru obstruktif kronik (PPOK) adalah penyakit paru obstruksi akibat proses inflamasi saluran pernapasan dan parenkim paru. Pada beberapa kasus PPOK ditemukan perubahan pada pembuluh darah pulmonal yang ternyata tidak jarang terjadi sehingga menyebabkan gangguan pertukaran gas dan menyebabkan hipertensi pulmonal yang berasosiasi dengan peningkatan morbiditas dan mortalitas (1,2). Menurut klasifikasi WHO terdapat 5 kelompok besar penyebab HP. Hipertensi pulmonal yang berhubungan dengan penyakit paru atau hipoksemia, termasuk PPOK masuk dalam kelompok ketiga <!--[if supportFields]>ADDIN CSL_CITATION { "citationItems" : [ { "id" : "ITEM-1", "itemData" : { "DOI" : "10.1161/CIRCULATIONAHA.109.192230", "ISSN" : "1524-4539", "PMID" : "19332472", "author" : [ { "dropping-particle" : "V", "family" : "McLaughlin", "given" : "Vallerie", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Archer", "given" : "Stephen L", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Badesch", "given" : "David B", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Barst", "given" : "Robyn J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Farber", "given" : "Harrison W", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Lindner", "given" : "Jonathan R", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Mathier", "given" : "Michael a", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "McGoon", "given" : "Michael D", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Park", "given" : "Myung H", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Rosenson", "given" : "Robert S", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Rubin", "given" : "Lewis J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Tapson", "given" : "Victor F", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Varga", "given" : "John", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Harrington", "given" : "Robert a", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Anderson", "given" : "Jeffrey L", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Bates", "given" : "Eric R", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Bridges", "given" : "Charles R", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Eisenberg", "given" : "Mark J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Ferrari", "given" : "Victor a", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Grines", "given" : "Cindy L", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Hlatky", "given" : "Mark a", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Jacobs", "given" : "Alice K", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Kaul", "given" : "Sanjay", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Lichtenberg", "given" : "Robert C", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Moliterno", "given" : "David J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Mukherjee", "given" : "Debabrata", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Pohost", "given" : "Gerald M", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Schofield", "given" : "Richard S", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Shubrooks", "given" : "Samuel J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Stein", "given" : "James H", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Tracy", "given" : "Cynthia M", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Weitz", "given" : "Howard H", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Wesley", "given" : "Deborah J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" } ], "container-title" : "Circulation", "id" : "ITEM-1", "issue" : "16", "issued" : { "date-parts" : [ [ "2009", "4", "28" ] ] }, "page" : "2250-94", "title" : "ACCF/AHA 2009 expert consensus document on pulmonary hypertension: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association: developed in collaboration with the American College ", "type" : "article-journal", "volume" : "119" }, "uris" : [ "http://www.mendeley.com/documents/?uuid=2f8ff7c0-0e3d-4d38-ac1d-1da69d1d66b5" ] } ], "mendeley" : { "previouslyFormattedCitation" : "(3)" }, "properties" : { "noteIndex" : 0 }, "schema" : "https://github.com/citation-style-language/schema/raw/master/csl-citation.json" }<![endif]-->(3)<!--[if supportFields]><![endif]-->.
Angka harapan hidup pasien PPOK yang disertai HP secara signifikan menurun dibandingkan pasien dengan PPOK atau HP yg tidak terjadi bersamaan. Tekanan arteri pulmonal adalah indikator paling baik untuk memprediksikan mortalitas. Angka harapan hidup 5 tahun pada pasien dengan mPAP>25 mmHg adalah 36% sedangkan pasien dengan mPAP kurang dari 25 mmHg meningkat menjadi 62%. Sementara itu tanda tanda disfungsi jantung kanan, tanda adanya hipertrofi ventrikel kanan pada EKG merupakan parameter lain yang berguna untuk memprediksikan angka harapan hidup <!--[if supportFields]>ADDIN CSL_CITATION { "citationItems" : [ { "id" : "ITEM-1", "itemData" : { "DOI" : "10.1183/09031936.00015608", "ISSN" : "1399-3003", "PMID" : "18978137", "abstract" : "Mild-to-moderate pulmonary hypertension is a common complication of chronic obstructive pulmonary disease (COPD); such a complication is associated with increased risks of exacerbation and decreased survival. Pulmonary hypertension usually worsens during exercise, sleep and exacerbation. Pulmonary vascular remodelling in COPD is the main cause of increase in pulmonary artery pressure and is thought to result from the combined effects of hypoxia, inflammation and loss of capillaries in severe emphysema. A small proportion of COPD patients may present with \"out-of-proportion\" pulmonary hypertension, defined by a mean pulmonary artery pressure >35-40 mmHg (normal is no more than 20 mmHg) and a relatively preserved lung function (with low to normal arterial carbon dioxide tension) that cannot explain prominent dyspnoea and fatigue. The prevalence of out-of-proportion pulmonary hypertension in COPD is estimated to be very close to the prevalence of idiopathic pulmonary arterial hypertension. Cor pulmonale, defined as right ventricular hypertrophy and dilatation secondary to pulmonary hypertension caused by respiratory disorders, is common. More studies are needed to define the contribution of cor pulmonale to decreased exercise capacity in COPD. These studies should include improved imaging techniques and biomarkers, such as the B-type natriuretic peptide and exercise testing protocols with gas exchange measurements. The effects of drugs used in pulmonary arterial hypertension should be tested in chronic obstructive pulmonary disease patients with severe pulmonary hypertension. In the meantime, the treatment of cor pulmonale in chronic obstructive pulmonary disease continues to rest on supplemental oxygen and a variety of measures aimed at the relief of airway obstruction.", "author" : [ { "dropping-particle" : "", "family" : "Chaouat", "given" : "a", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Naeije", "given" : "R", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Weitzenblum", "given" : "E", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" } ], "container-title" : "The European respiratory journal", "id" : "ITEM-1", "issue" : "5", "issued" : { "date-parts" : [ [ "2008", "11" ] ] }, "page" : "1371-85", "title" : "Pulmonary hypertension in COPD.", "type" : "article-journal", "volume" : "32" }, "uris" : [ "http://www.mendeley.com/documents/?uuid=5495390a-721f-4831-a61c-8a85b4340309" ] } ], "mendeley" : { "previouslyFormattedCitation" : "(4)" }, "properties" : { "noteIndex" : 0 }, "schema" : "https://github.com/citation-style-language/schema/raw/master/csl-citation.json" }<![endif]-->(4). Hipertensi pulmonal juga merupakan faktor prediktor kemampuan atau kapasitas olah raga (exercise capacity). Pada pasien dengan PPOK berat yang menjalani pemeriksaan kateterisasi jantung kanan ditemukan bahwa peningkatan mPAP berasosiasi dengan kemampuan test fisik yaitu 6 minutes walk distance (6MWD).
Hipertensi pulmonar tidak sama dengan hipertensi seperti biasanya. Pada kondisi hipertensi pulmonla arteri kecil di paru-paru menjadi sempit atau tersumbat. Lebih sulit bagi darah untuk mengalir melaluinya, dan ini dapat meningkatkan tekanan darah di paru-paru. Gejala hipertensi pulmonal biasanya tidak terlihat hingga kondisi berkembang. Gejala awal hipertensi pulmonal biasanya sesak napas dengan aktivitas sehari-hari, seperti menaiki tangga. Kelelahan, pusing, dan pingsan juga bisa menjadi gejala. Pembengkakan di pergelangan kaki, perut atau kaki, bibir dan kulit kebiruan, dan nyeri dada dapat terjadi saat tekanan pada jantung meningkat. Gejala berkisar dalam tingkat keparahan dan pasien tertentu mungkin tidak memiliki semua gejala.
Pada stadium lanjut, bahkan aktivitas minimal akan menghasilkan beberapa gejala seperti: detak jantung tidak teratur (palpitasi atau kuat, sensasi berdenyut), pingsan atau pusing, sesak napas progresif selama latihan atau aktivitas, serta kesulitan bernapas saat istirahat. Dengan mengenali gejala lebih awal kami mengharapkan para sobat sehat bisa membawa sanak keluarganya jika mengalami keluhan yang sama. Salam Sehat..Tetap Semangat
Referensi:
Elwing J, Panos RJ. Pulmonary hypertension associated with COPD. Int J Chron Obstruct Pulmon Dis.2008;3(1):55–70.
Jyothula S, Safdar Z. Update on pulmonary hypertension complicating chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2009;4:351–63.
McLaughlin V V, Archer SL, Badesch DB, Barst RJ, Farber HW, Lindner JR, et al. ACCF/AHA 2009 expert consensus document on pulmonary hypertension: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association: developed in collaboration with the American College . Circulation. 2019;119:2250–94.
Chaouat a, Naeije R, Weitzenblum E. Pulmonary hypertension in COPD. Eur Respir J. 2008;32:1371–85.