Mengenal Penyakit Hipertensi Pulmonal, Kenali Gejala Awalnya dan Terapinya, Fokus Pada Terapi Medikamentosa
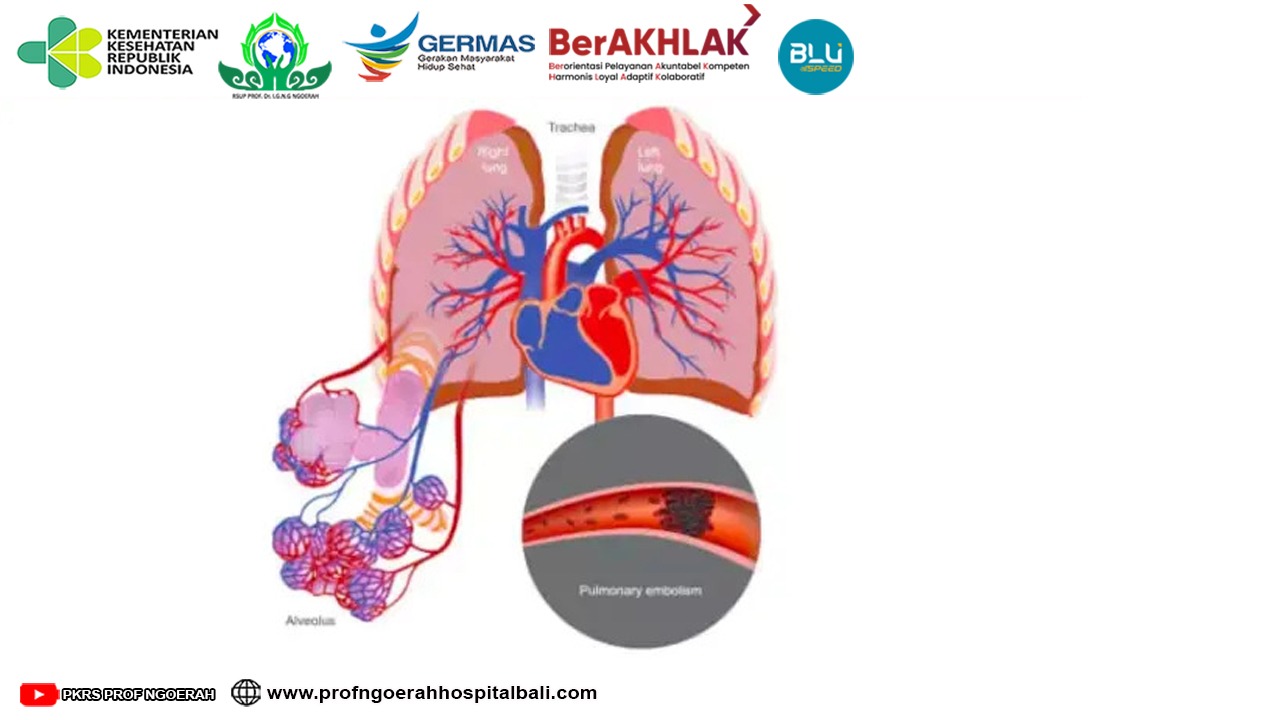
Optimalisasi penganganan PPOK sesuai guideline GOLD adalah kunci utama daripada penatalaksanaan umum. Asap rokok adalah penyebab paling sering terjadinya PPOK. Banyak penelitian melaporkan perbaikan gejala, fungsi paru, morbiditas dan mortalitas pasien PPOK setelah berhenti merokok <!--[if supportFields]>ADDIN CSL_CITATION { "citationItems" : [ { "id" : "ITEM-1", "itemData" : { "id" : "ITEM-1", "issued" : { "date-parts" : [ [ "0" ] ] }, "title" : "pathophysiology and clinical implication.pdf", "type" : "article" }, "uris" : [ "http://www.mendeley.com/documents/?uuid=99880bf6-a104-49a5-ba6e-83a6b929d156" ] } ], "mendeley" : { "previouslyFormattedCitation" : "(11)" }, "properties" : { "noteIndex" : 0 }, "schema" : "https://github.com/citation-style-language/schema/raw/master/csl-citation.json" }<![endif]-->(1)<!--[if supportFields]><![endif]-->. PPOK seperti pada pembahasan sebelumnya menjadi dasar munculnya kasus hipertensi pulmonal. Serta ada banyak metode untuk tata laksana dari gangguan ini, kali ini pembahasan akan menitikberatkan untuk tata laksana pengobatan (medikamentosa) sehingga kami berharap para sobat sehat mampu untuk memahaminya.
Calcium channel antagonist telah dievaluasi secara luas guna penanganan HP pada PPOK. Pemberian nifedipine dapat menurunkan mPAP dan meningkatkan CO pada pasien PPOK baik saat istirahat maupun aktivitas. Di lain pihak didapatkan bukti bahwa nifedipine menghambat hypoxic pulmonary vasoconstriction, sehingga memperburuk Va/Q dan menurunkan arterial oxygen tension (pO2). Penelitian klinis penggunaan calcium channel antagonist pada PPOK tidak menyebabkan perbaikan hemodinamik dan keadaan klinis. Data satu tahun terapi dengan angiotensin-II receptor antagonist juga tidak menunjukkan perbaikan mPAP atau kemampuan aktivitas pada pasien HP dengan PPOK. Secara keseluruhan dapat vasodilator sistemik pada PPOK dapat menurunkan mPAP dan meningkatkan CO tetapi dengan efek samping perburukan pertukaran gas. Pemberian vasodilator jangka panjang tidak disarankan karena tidak ada data yang mendukung <!--[if supportFields]>ADDIN CSL_CITATION { "citationItems" : [ { "id" : "ITEM-1", "itemData" : { "DOI" : "10.1183/09031936.94.07010148", "ISSN" : "00000000", "author" : [ { "dropping-particle" : "", "family" : "Weitzenblum", "given" : "E.", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Kessler", "given" : "R.", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Oswald", "given" : "M.", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Fraisse", "given" : "Ph.", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" } ], "container-title" : "European Respiratory Journal", "id" : "ITEM-1", "issue" : "1", "issued" : { "date-parts" : [ [ "1994", "1", "1" ] ] }, "page" : "148-152", "title" : "Medical treatment of pulmonary hypertension in chronic lung disease", "type" : "article-journal", "volume" : "7" }, "uris" : [ "http://www.mendeley.com/documents/?uuid=0a58957f-32f9-4af9-a82e-cb8e1a1bc114" ] }, { "id" : "ITEM-2", "itemData" : { "DOI" : "10.1161/CIRCULATIONAHA.109.192230", "ISSN" : "1524-4539", "PMID" : "19332472", "author" : [ { "dropping-particle" : "V", "family" : "McLaughlin", "given" : "Vallerie", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Archer", "given" : "Stephen L", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Badesch", "given" : "David B", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Barst", "given" : "Robyn J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Farber", "given" : "Harrison W", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Lindner", "given" : "Jonathan R", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Mathier", "given" : "Michael a", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "McGoon", "given" : "Michael D", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Park", "given" : "Myung H", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Rosenson", "given" : "Robert S", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Rubin", "given" : "Lewis J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Tapson", "given" : "Victor F", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Varga", "given" : "John", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Harrington", "given" : "Robert a", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Anderson", "given" : "Jeffrey L", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Bates", "given" : "Eric R", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Bridges", "given" : "Charles R", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Eisenberg", "given" : "Mark J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Ferrari", "given" : "Victor a", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Grines", "given" : "Cindy L", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Hlatky", "given" : "Mark a", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Jacobs", "given" : "Alice K", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Kaul", "given" : "Sanjay", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Lichtenberg", "given" : "Robert C", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Moliterno", "given" : "David J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Mukherjee", "given" : "Debabrata", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Pohost", "given" : "Gerald M", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Schofield", "given" : "Richard S", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Shubrooks", "given" : "Samuel J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Stein", "given" : "James H", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Tracy", "given" : "Cynthia M", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Weitz", "given" : "Howard H", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Wesley", "given" : "Deborah J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" } ], "container-title" : "Circulation", "id" : "ITEM-2", "issue" : "16", "issued" : { "date-parts" : [ [ "2009", "4", "28" ] ] }, "page" : "2250-94", "title" : "ACCF/AHA 2009 expert consensus document on pulmonary hypertension: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association: developed in collaboration with the American College ", "type" : "article-journal", "volume" : "119" }, "uris" : [ "http://www.mendeley.com/documents/?uuid=2f8ff7c0-0e3d-4d38-ac1d-1da69d1d66b5" ] }, { "id" : "ITEM-3", "itemData" : { "DOI" : "10.1513/pats.200407-037MS", "ISSN" : "1546-3222", "PMID" : "16113464", "abstract" : "Pulmonary hypertension is a common complication of chronic obstructive pulmonary disease (COPD). The increase in pulmonary artery pressures is often mild to moderate. However, 5-10% of patients with advanced COPD may suffer from severe pulmonary hypertension and present with a progressively downhill clinical course because of right heart failure added to ventilatory handicap. The prevalence of clinically significant severe pulmonary hypertension in COPD is roughly estimated to be of 1-2/1,000. The cause of pulmonary hypertension in COPD is generally assumed to be hypoxic pulmonary vasoconstriction leading to permanent medial hypertrophy. However, recent pathologic studies point rather at extensive remodeling of all layers of the pulmonary arterial walls. These aspects account for minimal reversibility with supplemental oxygen. There may be a case for pharmacologic treatment of pulmonary hypertension in selected patients with advanced COPD and right heart failure. However, it will be a challenge for randomized controlled trials to overcome the difficulties of the diagnosis of right ventricular failure and the definition of a relevant primary endpoint in pulmonary hypertensive patients with COPD.", "author" : [ { "dropping-particle" : "", "family" : "Naeije", "given" : "Robert", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" } ], "container-title" : "Proceedings of the American Thoracic Society", "id" : "ITEM-3", "issue" : "1", "issued" : { "date-parts" : [ [ "2005", "1" ] ] }, "page" : "20-2", "title" : "Pulmonary hypertension and right heart failure in chronic obstructive pulmonary disease.", "type" : "article-journal", "volume" : "2" }, "uris" : [ "http://www.mendeley.com/documents/?uuid=5c451c99-9fe6-4154-b35a-6cddf52dd61f" ] }, { "id" : "ITEM-4", "itemData" : { "ISSN" : "0021-8782", "PMID" : "12430958", "abstract" : "Chronic lung disease in humans is frequently complicated by the development of secondary pulmonary hypertension, which is associated with increased morbidity and mortality. Hypoxia, inflammation and increased shear stress are the primary stimuli although the exact pathways through which these initiating events lead to pulmonary hypertension remain to be completely elucidated. The increase in pulmonary vascular resistance is attributed, in part, to remodelling of the walls of resistance vessels. This consists of intimal, medial and adventitial hypertrophy, which can lead to encroachment into and reduction of the vascular lumen. In addition, it has been reported that there is a reduction in the number of blood vessels in the hypertensive lung, which could also contribute to increased vascular resistance. The pulmonary endothelium plays a key role in mediating and modulating these changes. These structural alterations in the pulmonary vasculature contrast sharply with the responses of the systemic vasculature to the same stimuli. In systemic organs, both hypoxia and inflammation cause angiogenesis. Furthermore, remodelling of the walls of resistance vessels is not observed in these conditions. Thus it has been generally stated that, in the adult pulmonary circulation, angiogenesis does not occur. Prompted by previous observations that chronic airway inflammation can lead to pulmonary vascular remodelling without hypertension, we have recently shown, using quantitative stereological techniques, that angiogenesis can occur in the adult pulmonary circulation. Pulmonary angiogenesis has also been reported in some other conditions including post-pneumonectomy lung growth, metastatic disease of the lung and in biliary cirrhosis. Such angiogenesis may serve to prevent or attenuate increased vascular resistance in lung disease. In view of these more recent data, the role of structural alterations in the pulmonary vasculature in the development of pulmonary hypertension should be carefully reconsidered.", "author" : [ { "dropping-particle" : "", "family" : "Hopkins", "given" : "Natalie", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "McLoughlin", "given" : "Paul", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" } ], "container-title" : "Journal of anatomy", "id" : "ITEM-4", "issue" : "4", "issued" : { "date-parts" : [ [ "2002", "10" ] ] }, "page" : "335-48", "title" : "The structural basis of pulmonary hypertension in chronic lung disease: remodelling, rarefaction or angiogenesis?", "type" : "article-journal", "volume" : "201" }, "uris" : [ "http://www.mendeley.com/documents/?uuid=c0d10e00-e761-4a77-acd5-523b0ce16d54" ] } ], "mendeley" : { "previouslyFormattedCitation" : "(3,12\u201314)" }, "properties" : { "noteIndex" : 0 }, "schema" : "https://github.com/citation-style-language/schema/raw/master/csl-citation.json" }<![endif]-->(2-4)<!--[if supportFields]><![endif]-->.
Nitric oxide (NO) sebagai vasodilator pembuluh darah paru selektif juga diteliti pada HP dengan PPOK. Inhalasi NO dosis rendah menurunkan mPAP tanpa mempengaruhi pertukaran gas normal. Jika diberikan dalam konsentrasi tinggi (40ppm), maka selain menurunkan mPAP juga akan memperburuk distribusi Va/Q dan PaO2. Pengaruh inhalasi NO dalam pertukaran gas ternyata lebih sedikit jika diberikan saat olah raga. Hal ini disebabkan karena pada aktivitas fisik didapatkan perbaikan ventilasi pada paru-paru sehingga pertukaran gas juga lebih efektiv. Yoshida et al. 2012 memaparkan bahwa pemberian kombinasi dosis rendah inhalasi NO (5 ppm) dan oksigen menghasilkan perbaikan hemodinamik dan oksigenasi yang lebih berarti dibandingan pemberian oksigen monoterapi. Pada RCT (40 pasien) dengan PPOK (FEV1 1,19+0,6L) dan HP (PAP>25 mmHg) menunjukkan penurunan mPAP dari 27,6 menjadi 20,6 mmHg (p kurang dari 0.001) etelah penggunaan kombinasi NO dan oksigen inhalasi. Terdapat pula penurunan pCO2 pada kelompok terapi yang membuktikan adanya perbaikan perfusi dan ventilasi.
Inhalasi iloprost memperbaiki ventilasi dan perfusi serta toleransi atau kemampuan aktivitas. Ini dibuktikan dengan perbaikan 6MWD 49,8+35 m (p kurang dari 0,02) (4,5)<!--[if supportFields]><![endif]-->. Keterbatasan iloprost adalah masa kerjanya yang pendek dan bertahan selama 2 jam. Sebagai alternatif adalah treprostinil yang mempunyai durasi kerja lebih panjang. Treprostinil (Remodulin) dapat diberikan intravena atau subkutan. Pemberian subkutan banyak dihindari oleh pasien karena nyeri di tempat suntik <!--[if supportFields]>ADDIN CSL_CITATION { "citationItems" : [ { "id" : "ITEM-1", "itemData" : { "DOI" : "10.1161/CIRCULATIONAHA.109.192230", "ISSN" : "1524-4539", "PMID" : "19332472", "author" : [ { "dropping-particle" : "V", "family" : "McLaughlin", "given" : "Vallerie", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Archer", "given" : "Stephen L", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Badesch", "given" : "David B", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Barst", "given" : "Robyn J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Farber", "given" : "Harrison W", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Lindner", "given" : "Jonathan R", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Mathier", "given" : "Michael a", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "McGoon", "given" : "Michael D", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Park", "given" : "Myung H", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Rosenson", "given" : "Robert S", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Rubin", "given" : "Lewis J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Tapson", "given" : "Victor F", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Varga", "given" : "John", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Harrington", "given" : "Robert a", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Anderson", "given" : "Jeffrey L", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Bates", "given" : "Eric R", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Bridges", "given" : "Charles R", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Eisenberg", "given" : "Mark J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Ferrari", "given" : "Victor a", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Grines", "given" : "Cindy L", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Hlatky", "given" : "Mark a", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Jacobs", "given" : "Alice K", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Kaul", "given" : "Sanjay", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Lichtenberg", "given" : "Robert C", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Moliterno", "given" : "David J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Mukherjee", "given" : "Debabrata", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Pohost", "given" : "Gerald M", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Schofield", "given" : "Richard S", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Shubrooks", "given" : "Samuel J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Stein", "given" : "James H", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Tracy", "given" : "Cynthia M", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Weitz", "given" : "Howard H", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Wesley", "given" : "Deborah J", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" } ], "container-title" : "Circulation", "id" : "ITEM-1", "issue" : "16", "issued" : { "date-parts" : [ [ "2009", "4", "28" ] ] }, "page" : "2250-94", "title" : "ACCF/AHA 2009 expert consensus document on pulmonary hypertension: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association: developed in collaboration with the American College ", "type" : "article-journal", "volume" : "119" }, "uris" : [ "http://www.mendeley.com/documents/?uuid=2f8ff7c0-0e3d-4d38-ac1d-1da69d1d66b5" ] }, { "id" : "ITEM-2", "itemData" : { "DOI" : "10.1093/eurheartj/ehp297", "ISSN" : "1522-9645", "PMID" : "19713419", "author" : [ { "dropping-particle" : "", "family" : "Gali\u00e8", "given" : "Nazzareno", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Hoeper", "given" : "Marius M", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Humbert", "given" : "Marc", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Torbicki", "given" : "Adam", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Vachiery", "given" : "Jean-Luc", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Barbera", "given" : "Joan Albert", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Beghetti", "given" : "Maurice", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Corris", "given" : "Paul", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Gaine", "given" : "Sean", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Gibbs", "given" : "J Simon", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Gomez-Sanchez", "given" : "Miguel Angel", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Jondeau", "given" : "Guillaume", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Klepetko", "given" : "Walter", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Opitz", "given" : "Christian", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Peacock", "given" : "Andrew", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Rubin", "given" : "Lewis", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Zellweger", "given" : "Michael", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" }, { "dropping-particle" : "", "family" : "Simonneau", "given" : "Gerald", "non-dropping-particle" : "", "parse-names" : false, "suffix" : "" } ], "container-title" : "European heart journal", "id" : "ITEM-2", "issue" : "20", "issued" : { "date-parts" : [ [ "2009", "10" ] ] }, "page" : "2493-537", "title" : "Guidelines for the diagnosis and treatment of pulmonary hypertension: the Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), endorsed by the Internat", "type" : "article-journal", "volume" : "30" }, "uris" : [ "http://www.mendeley.com/documents/?uuid=2f8f01e7-0e9d-443d-9b6b-3fe76c928849" ] } ], "mendeley" : { "previouslyFormattedCitation" : "(3,8)" }, "properties" : { "noteIndex" : 0 }, "schema" : "https://github.com/citation-style-language/schema/raw/master/csl-citation.json" }<![endif]-->(5,6)<!--[if supportFields]><![endif]-->.
Terapi kombinasi medikantosa dapat diberikan apabila terapi tunggal belum dapat memberikan efikasi yang baik. Tujuan terapi kombinasi adalah untuk mencapai efek pengobatan optimal dengan efek samping yang minimal yang biasanya dimulai pada pasien-pasien dengan WHO fungsional kelas III dan IV yang mengalami terapi refrakter dengan hanya 1 terapi. Sampai saat ini telah banyak dilakukan open label observational studies yang menunjukkan keuntungan terapi kombinasi ini (epoprostenol atau iloprost dengan bosentan, bosentan dan sildenafil, bosentan dan iloprost). Semoga informasi yang diberikan dapat bermanfaat bagi para sobat sehat.
Referensi:
Global Initiative for Chronic Obstructive Lung. 2023. http://www.goldcopd.org/guidelines-global-strategy-for-diagnosis-management.html
Stamm J a, Risbano MG, Mathier M a. Overview of current therapeutic approaches for pulmonary hypertension. Pulm Med.2011;1:138-59.
Naeije R. Pulmonary hypertension and right heart failure in chronic obstructive pulmonary disease. Proc Am Thorac Soc.2005;2:20–2.
Weitzenblum E, Kessler R, Oswald M, Fraisse P. Medical treatment of pulmonary hypertension in chronic lung disease. Eur Respir J.1994;7:148–52.
Hopkins N, McLoughlin P. The structural basis of pulmonary hypertension in chronic lung disease: remodelling, rarefaction or angiogenesis? J Anat. 2002;201:335–48.
Nef HM, Möllmann H, Hamm C, Grimminger F, Ghofrani H-A. Pulmonary hypertension: updated classification and management of pulmonary hypertension. Heart.2010;96:552–9